Background
DNA hypomethylating agents (HMAs), including azacytidine (AZA) have been established as key drugs for higher-risk myelodysplastic syndromes (MDS). We and others have explored the role of mutation profile before AZA administration on predicting outcomes. Actually, we have previously identified mutated-TP53 as a marker associated with higher rate of achieving complete remission (CR). In addition, mutations in TP53 and DDX41 predicted reduced and prolonged survival after treatment, respectively. However, the clinical significance of evaluating clone size changes early after treatment has not been determined. In this study, we explored the role of post-treatment clone size in predicting outcomes of AZA treatment for MDS and related diseases.
Methods
We enrolled 290 AZA-treated cases, including 88 from a Japanese prospective study (JALSG MDS-212 trial), 149 from Karolinska Institute, and 53 from a retrospectively collected Japanese cases. The diagnoses were MDS (n=242), MDS/MPN (n=25), and AML-MRC (n=23). For all patients, tumor samples were collected both before and after AZA administration and were analyzed for mutations in 66 genes implicated in myeloid neoplasms using targeted-capture sequencing. The median cycles of AZA treatment before sampling was 4 (range 1-7). Clone size was calculated from variant allele frequency adjusted for ploidy or allelic imbalances.Survival was calculated with a Cox regression model.
Results
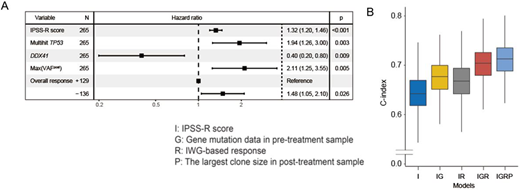
In post-treatment samples, we identified 870 mutations in 51 genes in 255 (88%) patients with a median of 3 mutations per sample, while 943 mutations were seen in 279 (96%) patients in the pre-treatment samples. Most frequently detected mutations in post-treatment samples were seen in TET2, TP53, RUNX1, and ASXL1. Germline DDX41 mutations were excluded from clone size evaluation. Median clone sizes were 0.63 and 0.54 for pre-treatment and post-treatment samples (P=.011), respectively. The largest clone sizes (max(VAF)) in post-treatment samples had a strong negative correlation with hematological response according to IWG criteria (P < .0001). We next explored whether max(VAF) in post-treatment samples provides a more precise estimation of long-term survival than IPSS-R. Max(VAF) further stratified each IPSS-R risk group in subgroups with discrete OS (P < .0001 for IPSS-R very high and P = .0004 for high risk group). Incorporating pre-treatment mutation data (mutations in TP53 and DDX41) and max(VAF) values in addition to IPSS-R scores and clinical response, we constructed a multivariate model and found that all these factors had an independent and significant impact on OS (Figure 1A). Next, we examined whether max(VAF) combined with IPSS-R and clinical response can improve the model. For this purpose, we randomly split the cohort into 75% training and 25% validation subsets and for each split, we constructed different models using the training set, performance of which was evaluated by calculating the concordance index (c-index) using the validation set. The mean c-index in 10,000 simulation sets increased by 0.025 by adding response data to IPSS-R score (I versus IR in Fig 1B). Further improvements were obtained by adding gene mutation and max(VAF), in which the c-index increased by 0.034 (IR versus IGR in Fig 1B) and 0.010 (IGR versus IGRP in Fig 1B), respectively. For the 53 patients who received allogeneic stem cell transplantation, the median post-transplant OS was 82.6 months (range, 36.3 to not reached). Notably, max(VAF) significantly stratified OS after allo-SCT (HR, 3.3; 95%CI, 1.3 to 8.3; P = .014).
Conclusions
Our study revealed that post-treatment clone size significantly correlated with clinical response and the evaluation of post-treatment clone size allows for more precise prognostication after AZA treatment compared with IPSS-R and clinical response alone.
Naoe:NIPPON SHINYAKU CO.,LTD.: Speakers Bureau; Sysmex co.: Speakers Bureau; Eisai Co., Ltd.: Speakers Bureau; Astellas Pharma Inc.: Speakers Bureau; Bristol-Myers Squibb Company: Speakers Bureau. Miyazaki:Celgene: Honoraria; Sumitomo Dainippon Pharma Co., Ltd.: Honoraria; Kyowa Kirin Co., Ltd.: Honoraria; Novartis Pharma KK: Honoraria; NIPPON SHINYAKU CO.,LTD.: Honoraria; Otsuka Pharmaceutical: Honoraria; Astellas Pharma Inc.: Honoraria; Chugai Pharmaceutical Co., Ltd.: Honoraria. Papaemmanuil:Kyowa Hakko Kirin: Consultancy, Honoraria; Prime Oncology: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; Illumina: Consultancy, Honoraria; Celgene: Consultancy, Honoraria, Research Funding; MSKCC: Patents & Royalties; Isabl: Current equity holder in private company, Membership on an entity's Board of Directors or advisory committees. Ogawa:Eisai Co., Ltd.: Research Funding; Chordia Therapeutics, Inc.: Membership on an entity's Board of Directors or advisory committees, Research Funding; KAN Research Institute, Inc.: Membership on an entity's Board of Directors or advisory committees, Research Funding; Otsuka Pharmaceutical Co., Ltd.: Research Funding; Asahi Genomics Co., Ltd.: Current equity holder in private company; Sumitomo Dainippon Pharma Co., Ltd.: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.